New lungs, new life
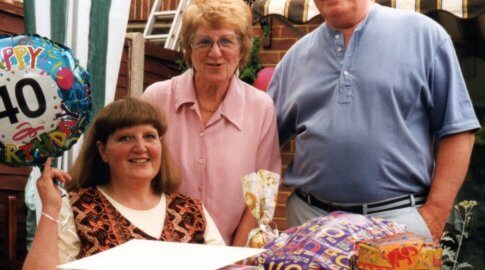
Young teenager Charlie Beeton received a double lung transplant just a few months after being diagnosed with PH – and celebrated his 13th birthday in hospital just nine days later. Here, his mother Claire shares the story of his remarkable recovery.

We had never heard of pulmonary hypertension before Charlie’s diagnosis in September 2017. The amazing paediatrician at our local hospital in Bedford knew exactly what he was looking at as soon as he had completed the ultrasound but didn’t go in to a great deal of detail at that point (for which I am very grateful). He did get Charlie onto the ward and hooked up to oxygen immediately, and we saw the improvement in his appearance straight away.
We knew that we were to be transferred to Great Ormond Street Children’s Hospital quickly and it was once we were there that Charlie really started to deteriorate. We were immediately introduced to the transplant team. I was in equal parts devastated at the seriousness and severity of Charlie’s condition, and relieved that we were finally dealing with a definite ‘thing’. We knew that we were in the care of the best people and that whatever the outcome, it would be the best it could be.
Charlie was on the transplant list for just two months.
We were advised that because of his blood type donor organs were easier to match to him and that it would be fairly quick – we weren’t expecting it to be that quick though! In those two months we were called into hospital twice with possible matches before that third and final call that ended in a very successful transplant.
The incredibly quick turnaround of just four months from diagnosis to transplant really didn’t leave much ‘coping’ time at all. I have not had the opportunity to speak to other families who have experienced a child or other relative being on a transplant waiting list, but I would imagine that our situation is quite unusual.
At the time of Charlie’s transplant, we were still in shock and if I am to be perfectly honest it was hard to celebrate it in the same way that a family who has endured a long and arduous wait might.
Although vastly improved by the constant epoprostenol (epo) infusion, Charlie was still very poorly and we simply couldn’t envisage anything beyond him being wheeled in to theatre. We knew that he was in amazing hands, that the surgical team were world class and that Charlie would not have been listed in the first place if they were not confident of a successful outcome, but we couldn’t imagine anyone surviving that operation.
To say that Charlie is a different child post-transplant would be the understatement of the century!
He looked better that he had in years immediately after coming out of surgery, despite all the tubes and gubbins. He was lovely and pink! He was out of bed within 36 hours, outside of the hospital for a wander about in a week and home on the mainline train just two weeks post-surgery.

He has continued his recovery without a single setback; not a cold, a sickness bug or any time off school at all, apart from for clinic appointments.
It took Charlie a long time to realise how very poorly he had been; he had just adapted to his failing health as the years had gone by. His acceptance that he was in fact ill, and that he does in fact now feel much better, has been key in his continued improvement.
He just has so much more ‘about’ him now. It is not just his energy, fitness and improved physical health and appearance. It is his amazing personality that is growing all the time.
He is enjoying life so much more now, as are all of us. We had not realised how much we were missing out on as a family before Charlie’s diagnosis and subsequent treatment.
Claire Beeton
Charlie developing idiopathic pulmonary hypertension is devastating, but that’s our lot, and we must accept it.
We count ourselves as so incredibly lucky that it was diagnosed and treated in time, and that we are currently enjoying the most ‘normal’ and happy times as a family that we have ever wished for.
Claire’s advice for other parents
- We were very busy with clinic appointments, medicine deliveries, visits from the community nurses and goodness knows what else. I tracked down online and printed off an A4 week-to-view calendar. Lots of room to write everything clearly, and there really was something to deal with most days.
- It helped us to keep all correspondence, discharge letters and appointment letters in a folder just for Charlie.
- If your child is about to begin using the epo, do not underestimate how much room the medicine, syringes, needles, pumps and goodness-knows-what-else will take up in your home!
- We were advised by another parent to invest in a baby monitor to help us if the CADD pump went off overnight. I am really pleased to say that we did not have any problems with any of the pumps at all, but it was good to have that as a back-up just in case.