Long Acting reversible Contraception (LARCS)
This group of contraceptives includes implants, injections and coils (or Intra-Uterine Devices and Intra-uterine systems). None of these methods depend on you remembering to take or use them to work which makes them highly effective. In fact, LARCs have a lower failure rate than female sterilisation, yet they are fully reversible with fertility returning once they stop being used.
Contraceptive implants
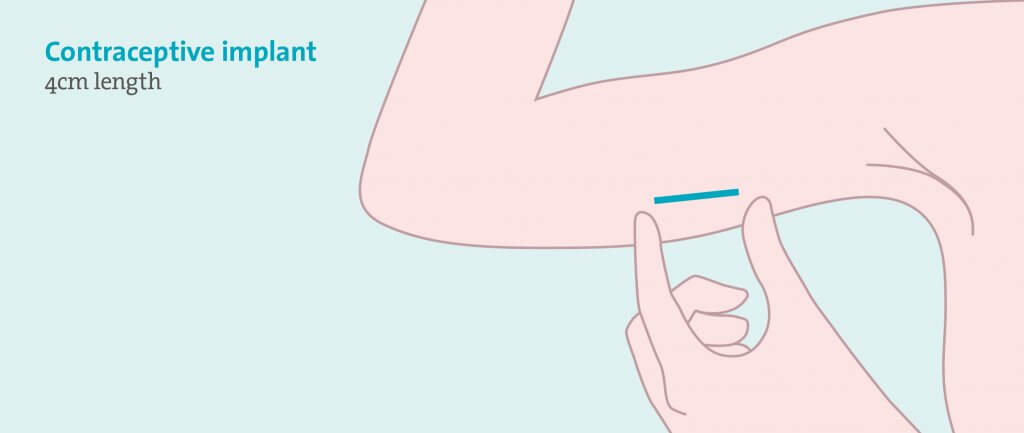
What it is and how it works
An implant is a small rod, about the size of a matchstick. It is inserted into the upper arm, just under the skin, with the use of a local anaesthetic. The rod steadily releases a hormone similar to progestogen, called etonogestrel, and each rod contains enough of the hormone to last for three years. The etonogestrel works in three ways: by stopping ovulation, by thickening the cervical mucus to stop the sperm reaching the egg, and by thinning the lining of the womb to prevent a fertilised egg implanting.
How effective is it?
Implants are very effective-over 99%. This means that less than one implant user in 100 will get pregnant in one year. When the implant is used for three years, less than one implant user in every 1,000 will get pregnant over three years.
Pros and cons
The positive reasons for choosing this as a method of contraception are that it is simple to have one fitted; once fitted, you don’t have to remember to use it, it just steadily works away in the background, and because it doesn’t rely on you remembering to use it, it is really effective. Once the rod is removed, the contraceptive effect immediately stops working.
The side effects from the implant are broadly split into two groups; how the hormone, etonogestrel, makes you feel and how the it affects your periods. The etonogestrel released from the implant can produce unwanted effects such as headaches, acne, breast tenderness and mood changes, a little bit like you feel the week before your period. These effects tend to wear off as your body gets used to the different hormone levels. It can also lead to a change in your periods; often they become lighter or absent altogether which is not always a bad thing. Sometimes though, bleeding can become heavier or more prolonged. If this does happen, additional medication can be taken to try and control the bleeding and it will often settle down within 6 months of having the implant inserted.
Relevance in PH
For women with PH, the implant provides effective and rapid protection from pregnancy with only the need for a local anaesthetic.
Q. Is the implant affected by my PH drugs?
The only PH drug which has the potential to interact with the implant is Bosentan, an Endothelin Receptor Agonist. It is thought Bosentan makes the implant less effective, so if you are on this drug as part of your PH medication, you will need to consider a second contraceptive as well as the implant.
Q. Does the implant provide contraception straight away?
If the implant is fitted within 5 days after your period starts, it will provide contraception straight away. If you have it fitted at any other time of your monthly cycle, it will not guarantee protection from pregnancy for 7 days. During these 7 days you will need to use another form of contraception, eg a condom.
Q. I’m a bit nervous about having an implant in. What happens if it doesn’t suit me?
It is always worth giving any new form of contraception 6 months before deciding it isn’t the right one for you. It can take as long as this for the body to adapt to the different levels of hormones. If, after this time, it still is not suiting you, then it is a simple procedure to remove the implant, making sure you had other contraceptives in place.
Contraceptive injections
What it is and how it works
There are three types of contraceptive injections, Depo-Provera, Sayana Press and Noristerat. Depo-Provera is an injection of a hormone similar to progesterone, called medroxyprogesterone acetate. It is given into a large muscle, for example a buttock or an upper arm muscle, and one dose lasts for 13 weeks. Sayana Press also contains the hormone medroxyprogesterone acetate but in a slightly lower dose. It is injected beneath the skin, normally on the abdomen or upper thighs, and one dose also lasts for 13 weeks. Noristerat is an injection of a hormone called norethisterone enantate, again a hormone very similar to progesterone. It is given into a large muscle, normally the buttocks, and one dose lasts for 8 weeks only. It is also a thicker solution so can be more uncomfortable when injected. This injection is not commonly used in the UK.
The above injections all work in the same way: by stopping ovulation, by thickening the cervical mucus to stop the sperm reaching the egg, and by thinning the lining of the womb to prevent a fertilised egg implanting.
How effective is it?
If used perfectly, injections can be very effective- over 99%. However, because the 12-week (or 8-week) window can be missed, typical use is not quite as effective with figures suggesting that around 6 in 100 women using contraceptive injections will get pregnant in one year.
Pros and cons
This is an effective form of contraception that you don’t have to remember to use on a daily basis. It is just one simple injection which lasts for 12 (or 8) weeks.
The unwanted effects are similar to the implant and again come from the different levels of hormones circulating your body. Side effects include headaches, acne, breast tenderness and mood changes. The injections can affect your periods too; they can become lighter or absent altogether or can become more frequent and heavier. One significant side effect which is different to other long acting contraceptives, is that with the injections, fertility can take longer to return to normal after you stop them (up to a year).
Relevance in PH
For women with PH, the contraceptive injection can provide effective protection from pregnancy, but it is worth noting that it lasts for the shortest amount of time
compared with others in this group. If you have PH, the chances are you already have to factor in outpatient appointments on a fairly regular basis and to have to book another appointment every 12 weeks on top may just feel like one appointment too far.
Q. Do my PH drugs interact with the contraceptive injection?
The only PH drug which has the potential to interact with the contraceptive injection is Bosentan, an Endothelin Receptor Agonist. It is thought Bosentan makes the injection less effective, so if you are on this drug as part of your PH medication, you will need to consider a second contraceptive as well as the implant.
Q. Does the injection provide contraception straight away?
If the injection is given within 5 days of your period starting, it will provide contraception straight away. If you have it at any other time of your monthly cycle, it will not guarantee protection from pregnancy for 7 days. During these 7 days you will need to use another form of contraception, eg a condom.
Q. I can’t decide between the injection and the implant. I don’t like the idea of having to have injections every 12 weeks but I’m nervous of having something fitted that lasts for three years without knowing if it suits me.
One thing that can be helpful before having an implant fitted, is to try using the contraceptive injection for 6-12 months. Women who have few problems with the injection, are likely to have very few problems with the implant too.
Intra-uterine devices (IUDs)
What it is and how it works
Commonly referred to as coils, these are small plastic and copper devices. They are put into the uterus (womb) through the cervix (the neck of the womb). The copper prevents sperm from surviving and alters the cervical mucus to prevent sperm from reaching an egg. An IUD may also stop a fertilised egg implanting in the uterus. It is a simple procedure to insert an IUD but does require an internal examination. It can be a little uncomfortable but generally does not require any anaesthetic. Once inserted they last from 5 to 10 years depending on the type.
How effective is it?
IUDs are over 99% effective; which means that less than one IUD user in 100 will get pregnant in one year. When considering a 5-year time frame, less than 2 in 100 IUD users will get pregnant over this duration.
Pros and cons
An IUD provides instant protection from pregnancy and, once fitted, it can stay there a long time with very little attention. It doesn’t rely on you remembering to use it which makes it a very effective form of contraception. It contains no hormones, so it can be useful if you are particularly sensitive to hormones used in other contraceptives.
The most common unwanted effects from an IUD is an increase in menstrual bleeding; this can be quite significant.
Relevance in PH
For women with PH, an IUD gives instant, reliable contraception. It doesn’t contain any hormones so there are no interactions with any medications you may be taking.
Q. My mum says I shouldn’t have a coil because I have never been pregnant. Why does she think this?
In the past, the advice was only to use coils in women who had already had children. However over recent years research has shown that an IUD is a safe and effective form of contraception for women who have never been pregnant.
Q. I have heard you can catch infections from the coil. Is this right?
Having an IUD in place does not cause sexually transmitted infections or mean you are more likely to catch an infection, but if an infection is caught, it can spread up into the pelvis more easily which has the potential to cause long term problems. This is why you have to be more careful regarding sexually transmitted infections when using the IUD.
Q. I’m thinking of using the coil but I take warfarin. Would this be a good contraception for me to use?
One draw-back with the IUDs can be heavy menstrual bleeding. If you are taking any type of blood thinners because of your PH, it is probably worth considering an IUS instead of an IUD (see section below).
Intra-uterine systems (IUS)
What it is and how it works
An IUS is a small plastic device which is inserted into the uterus (womb) through the cervix (the neck of the womb). It has a coating on it which slowly releases a hormone called levonorgestrel, similar to progestogen. The IUS works by thinning the lining of the womb to prevent a fertilised egg implanting, by thickening the cervical mucus to stop the sperm reaching the egg and, in some people, it actually stops ovulation. The amount of hormone released is much smaller than in the contraceptive injection and implant and most of it only acts locally in the womb rather than getting into the bloodstream and affecting the whole body. The insertion of an IUS is a simple procedure but still requires an internal examination. It can be a little uncomfortablebut generally does not require any anaesthetic. Once inserted they last from 3 to 5 years depending on the type of IUS.
How effective is it?
IUS’s are over 99% effective; which means that less than one IUS user in 100 will get pregnant in one year.
Pros and cons
An IUS gives instant and reliable contraception. You don’t have to remember to use it and it provides contraceptive cover for a long time with very little attention. The hormone it releases acts locally, so there are no side effects affecting the rest of the body. Because of the addition of the hormone to the coil, it can incredibly useful for women with heavy periods- in fact it is used as treatment for heavy menstrual bleeding alone, even if contraception isn’t needed.
The most common side effects from an IUS that can be troublesome are a change in a woman’s periods. The first 6 months after an IUS is inserted, it is common to get irregular bleeding or spotting. This tends to settle down and most women find that their periods are lighter and shorter or even that they stop altogether.
Relevance in PH
For women with PH, an IUS is a useful form of contraception worth considering. There is no need to worry about interactions with any medications you may be taking, as the hormone released only acts within the womb.
Q. My friend had her coil fitted by her GP. Will I be able to get one fitted at my GP surgery?
It is probably worth discussing with your local PH team where the best place is for you to have a coil fitted. Inserting a coil is a simple procedure which only takes about 5-10 minutes. However, passing a coil through the neck of the womb can sometimes cause a vasovagal reaction (a simple fainting reaction) which can cause changes in your blood pressure and heart rate. It is not necessarily more likely to happen in women with PH, but if it does, it can have more of an effect.
Q. I have heard people have problems with coil threads. What are they and what problems can they cause?
Both an IUS and an IUD have two fine threads attached to them. After the device is inserted into the womb, the fine threads trail out of the cervix. After insertion, the threads are cut to about 2-3cm in length. They are important in being able to remove the device when needed and are also helpful in checking that the device is still in place. Sometimes, partners report they can feel the threads during sex. This is uncommon and if it happens you should see a GP or a nurse for a check-up to see if the device is in the right place or if the threads are a little on the long side.
Q. I have heard you can catch infections from the coil. Is this right?
Having an IUS in place does not cause sexually transmitted infections or mean you are more likely to catch an infection, but if an infection is caught, it can spread up into the pelvis more easily which has the potential to cause long term problems. This is why you have to be more careful regarding sexually transmitted infections when using the IUS.